Quiz-summary
0 of 9 questions completed
Questions:
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
Information
Additional questions for practice.
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 9 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
| Average score |
|
| Your score |
|
Categories
- Acyanotic CHD 0%
- Arrhythmia 0%
- Cardiomyopathy 0%
- Clinical Presentation 0%
- Connective tissue disorder 0%
- Cyanotic CHD 0%
- Dyslipidemia 0%
- Infection/Vasculitis 0%
| Pos. | Name | Entered on | Points | Result |
|---|---|---|---|---|
| Table is loading | ||||
| No data available | ||||
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- Answered
- Review
-
Question 1 of 9
1. Question
1 pointsA ten year-old male patient presents to his pediatrician’s office for a regular checkup. His past medical history is remarkable for occasional headaches, but the patient otherwise has no complaints. On physical Examination, Initial vital signs are notable for elevated blood pressure (154/78 mmHg) in the right upper extremity. In general, the patient is well-developed and well-appearing, in no acute distress. Cardiac examination is notable for weak femoral pulses bilaterally. On auscultation, the patient is noted to have a 3/6 systolic murmur in the left infra-clavicular area. On recheck of the patient’s triage vital signs, the patient is noted to have a blood pressure of 157/79 in the upper extremity and 109/60 mmHg in the lower extremity.
The best next step in management of this young man is:
Correct
That is Correct!
This patient is presenting with hypertension and headaches. The differential diagnosis for hypertension includes essential hypertension, endocrine disorders, renovascular disease, or cardiac causes such as coarctation of the aorta or conditions associated with a large stroke volume, the differential blood pressure between upper and lower extremities strongly suggests coarctation of the aorta. Transthoracic Echocardiography is indicated in this case to confirm the suspected diagnosis of coarctation of the aorta. Transthoracic echocardiography can also rule in or out other associated cardiac defects, including bicuspid aortic valve and ventricular septal defect. The best treatment option for this patient, giving his old age, is percutaneous balloon angioplasty of the coarctation area with stent placement.
SOURCE:
Coarctation of the aorta by Sawsan Awad and Megan McCarville. Chapter 12, page: 159-166. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.Incorrect
The correct answer is D.
This patient is presenting with hypertension and headaches. The differential diagnosis for hypertension includes essential hypertension, endocrine disorders, renovascular disease, or cardiac causes such as coarctation of the aorta or conditions associated with a large stroke volume, the differential blood pressure between upper and lower extremities strongly suggests coarctation of the aorta. Transthoracic Echocardiography is indicated in this case to confirm the suspected diagnosis of coarctation of the aorta. Transthoracic echocardiography can also rule in or out other associated cardiac defects, including bicuspid aortic valve and ventricular septal defect. The best treatment option for this patient, giving his old age, is percutaneous balloon angioplasty of the coarctation area with stent placement.
SOURCE:
Coarctation of the aorta by Sawsan Awad and Megan McCarville. Chapter 12, page: 159-166. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011. -
Question 2 of 9
2. Question
1 pointsA ten day old newborn presents to the emergency room with increased irritability and poor feeding in the last 2-3 days. He was born full term via normal vaginal delivery with no history of complications during pregnancy. He did well in the first week of life, but started to have episodes of intermittent irritability and decreased oral intake in the last 3 days with noticeable ashen discoloration of his skin. Mother denies fever, vomiting, diarrhea or history of illnesses with other family members. On examination, the patient is awake but has decreased activity with stimulation. Heart rate is 180 bpm, respiratory rate 40, and oxygen saturation is 95% on room air. On cardiac examination, no murmurs were detected. However, pulses were markedly diminished in all 4 extremities with reduced capillary refill (4 seconds).
The best next step in management of this newborn is:Correct
That is Correct!
This infant is demonstrating signs of acute circulatory shock, without respiratory distress. His clinical picture is suggestive of a left heart obstructive lesion, including subaortic obstruction secondary to hypertrophic cardiomyopathy and septal hypertrophy, critical aortic stenosis, coarctation of the aorta, interrupted aortic arch, or hypoplastic left heart syndrome. The onset of clinical presentation in this age is consistent with the closure of the PDA. Other causes of cardiogenic shock such as sepsis should also be considered but not to be the only diagnosis.
IV fluid bolus may provide temporary improvement of the patient’s clinical status due to increase intravascular volume that forces the small closing PDA to temporary open.
Prostaglandin should be started upon suspecting left sided cardiac obstructive lesion to maintain patency of the ductus arteriosus resulting in improvement of systemic perfusion. Echocardiography is an essential tool in confirming the diagnosis but initiation of PGE 2 should not be delayed until obtaining the TTE. Given the early onset of symptom in neonatal period, surgery with resection of the coarctation
segment and end-to-end anastomosis of the aortic segments is the best intervention once the child is stabilized from clinical point of view.SOURCE:
Coarctation of the aorta by Sawsan Awad and Megan McCarville. Chapter 12, page: 159-166. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.Incorrect
The correct answer is C.
This infant is demonstrating signs of acute circulatory shock, without respiratory distress. His clinical picture is suggestive of a left heart obstructive lesion, including subaortic obstruction secondary to hypertrophic cardiomyopathy and septal hypertrophy, critical aortic stenosis, coarctation of the aorta, interrupted aortic arch, or hypoplastic left heart syndrome. The onset of clinical presentation in this age is consistent with the closure of the PDA. Other causes of cardiogenic shock such as sepsis should also be considered but not to be the only diagnosis.
IV fluid bolus may provide temporary improvement of the patient’s clinical status due to increase intravascular volume that forces the small closing PDA to temporary open.
Prostaglandin should be started upon suspecting left sided cardiac obstructive lesion to maintain patency of the ductus arteriosus resulting in improvement of systemic perfusion. Echocardiography is an essential tool in confirming the diagnosis but initiation of PGE 2 should not be delayed until obtaining the TTE. Given the early onset of symptom in neonatal period, surgery with resection of the coarctation
segment and end-to-end anastomosis of the aortic segments is the best intervention once the child is stabilized from clinical point of view.SOURCE:
Coarctation of the aorta by Sawsan Awad and Megan McCarville. Chapter 12, page: 159-166. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011. -
Question 3 of 9
3. Question
1 pointsA 3 month old boy was seen by a pediatrician for the first time. The child was brought for a well child care visit; however, the mother did have concerns regarding bluish discoloration of the lips when he cries. On physical examination the heart rate was 110 bpm, regular. Respiratory rate was 35/minute. Blood pressure in upper extremity was 90/60 mmHg. Oxygen saturation was 88% in upper and lower extremity. Weight was at 5th percentile and height was at 25th percentile on the growth chart. The child appeared to have mild increase in respiratory effort with noticeable intercostal retractions. Peripheral pulses and perfusion were normal. Mild Hepatomegaly was detected. The precordium was clearly hyperactive with a palpable thrill. On auscultation, S1 and S2 were normal with a harsh 4/6 systolic ejection murmur detected over the left upper sternal border.
The most likely diagnosis of this toddler is:Correct
That is Correct!
History is significant for bouts of cyanosis with agitation. That points to base line desaturation that is not obvious by inspection during rest. That subsequently decreases with agitation due to increase pulmonary vascular resistance. The child apparently has a mild oxygen desaturation (88%) which should not cause obvious cyanosis upon inspection. Single ventricle lesions are a group of congenital heart disease that are cyanotic and come in different anatomical arrangement. The case in hand is a single RV, hypo-plastic, atretic, LV and normally related great arteries with mild to moderate pulmonary valve stenosis. The base line cyanosis is secondary to mixed blood (fully saturated blood rom left atrium and desaturated blood from the right atrium mix in the single ventricle). Increase in pulmonary blood flow result in lessening the extent of cyanosis, however, at the expense of pulmonary edema. This child does have pulmonary edema and congestive heart failure, however, mild. The cyanotic congenital heart disease this child has is well balanced. Cyanosis is mild and congestive heart failure has not resulted in significant symptoms.
The harsh systolic ejection murmur over the pulmonic area clearly points to a cardiac abnormality, likely involving the pulmonary valve. Although cyanosis causes increase respiratory effort, the mild oxygen desaturation noted is unlikely the culprit to increase in respiratory effort, which is most probably due to associated increase in pulmonary blood flow and edema.
ASD is not the correct choice as it is one of the acyanotic CHD, unless associated with other complex cardiac lesions. Coarctation of the aorta is less likely giving normal pulses and perfusion. D-TGA , although a cyanotic CHD, is not the correct answer. D-TGA patients present in newborn period and they are extremely sick. Almost none of patients with D-TGA will survive without any intervention to be 3 months old. Ventricular septal defect is not the correct answer either. It is one of the acyanotic CHD. VSD patients may present with cyanosis when they have long standing VSD with significant pulmonary hypertension and reversal of the shunt across the VSD from being left to right to be right to left. This entity is called Eisenmenger’s syndrome and doesn’t usually present that early. Its usual presentation is in late tents early twenties and beyond.
The child in the question continued follow up with pediatric cardiology after initiating anti-congestive heart failure medications including furosemide and after load reducing agent. The child was subsequently scheduled for cardiac catheterization to assess pulmonary vascular resistance prior to undergoing Glenn shunt at 3-6 months of age.SOURCE:
Single Ventricle by Sawsan Awad and Ra-id Abdulla. Chapter 21, page: 249-256. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.Incorrect
The correct answer is B.
History is significant for bouts of cyanosis with agitation. That points to base line desaturation that is not obvious by inspection during rest. That subsequently decreases with agitation due to increase pulmonary vascular resistance. The child apparently has a mild oxygen desaturation (88%) which should not cause obvious cyanosis upon inspection. Single ventricle lesions are a group of congenital heart disease that are cyanotic and come in different anatomical arrangement. The case in hand is a single RV, hypo-plastic, atretic, LV and normally related great arteries with mild to moderate pulmonary valve stenosis. The base line cyanosis is secondary to mixed blood (fully saturated blood rom left atrium and desaturated blood from the right atrium mix in the single ventricle). Increase in pulmonary blood flow result in lessening the extent of cyanosis, however, at the expense of pulmonary edema. This child does have pulmonary edema and congestive heart failure, however, mild. The cyanotic congenital heart disease this child has is well balanced. Cyanosis is mild and congestive heart failure has not resulted in significant symptoms.
The harsh systolic ejection murmur over the pulmonic area clearly points to a cardiac abnormality, likely involving the pulmonary valve. Although cyanosis causes increase respiratory effort, the mild oxygen desaturation noted is unlikely the culprit to increase in respiratory effort, which is most probably due to associated increase in pulmonary blood flow and edema.
ASD is not the correct choice as it is one of the acyanotic CHD, unless associated with other complex cardiac lesions. Coarctation of the aorta is less likely giving normal pulses and perfusion. D-TGA , although a cyanotic CHD, is not the correct answer. D-TGA patients present in newborn period and they are extremely sick. Almost none of patients with D-TGA will survive without any intervention to be 3 months old. Ventricular septal defect is not the correct answer either. It is one of the acyanotic CHD. VSD patients may present with cyanosis when they have long standing VSD with significant pulmonary hypertension and reversal of the shunt across the VSD from being left to right to be right to left. This entity is called Eisenmenger’s syndrome and doesn’t usually present that early. Its usual presentation is in late tents early twenties and beyond.
The child in the question continued follow up with pediatric cardiology after initiating anti-congestive heart failure medications including furosemide and after load reducing agent. The child was subsequently scheduled for cardiac catheterization to assess pulmonary vascular resistance prior to undergoing Glenn shunt at 3-6 months of age.SOURCE:
Single Ventricle by Sawsan Awad and Ra-id Abdulla. Chapter 21, page: 249-256. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011. -
Question 4 of 9
4. Question
1 pointsA 16-year-old female was referred to the cardiology clinic by her primary care physician. She had history of sore throat, and fever for 3 weeks. A few days ago, she started to have joint pains and swelling and felt progressively tired over the past few days. Joint pain, swelling and redness was first experienced in the right knee and resolved just as she was experiencing similar symptoms in the left knee. There was noticeable redness and swelling of the left knee joint. The right knee appeared to be within normal limits. Cardiac examination revealed distant S1, and S2 with a 3/6 holo-systolic murmur heard best over the apical region; in addition, a 1-2/4 diastolic murmur was heard over the apical region. Abdominal examinations revealed mild hepatomegaly. Transthoracic echocardiography revealed dilated left ventricle with mildly decreased systolic function. The mitral valve leaflets were thickened with moderate to severe regurgitation. Trivial aortic regurgitation was noted. In addition, mild to moderate pericardial effusion was present.
In addition to this patient’s findings, the following criteria are needed to make the diagnosis of rheumatic hear disease:Correct
That is Correct!
This patient manifested 2 major Jones criteria: polyarthritis and carditis, thus satisfying criteria for the diagnosis of rheumatic fever and rheumatic heart disease but missing an evidence of GAS infection. That can be documented by detecting an elevated acute phase reactant (ASOT). The time lapse between sore throat and the onset of the symptoms is consistent with the diagnosis of rheumatic fever. The migratory nature of polyarthritis in this patient is consistent with rheumatic fever. Carditis in this patient involves valve lesion (mitral regurgitation), myocardial affliction (poor myocardial function) and pericardial disease (pericardial effusion). Progressive fatigue and enlarged liver are manifestations of heart failure.
Chorea alone, without any other manifestation is satisfactory of diagnosing RF/RHD. Chorea usually is not associated with any other manifestations of RF. SC nodules is another major Jones criteria. Its presence in addition of the already present 2 major jones criteria in this patient is not confirmatory of RF without the presence of elevated acute phase reactant.
Skin rash in general is not diagnostic for RF. The particular rash of RF is the erythema marginatum. Even if this is present, as the SC nodules cannot complete the diagnosis of RF without elevated acute phase reactant.
Prolonged PR interval on 12 lead ECG together with fever are minor Jones criteria of RF.SOURCE:
Rheumatic Fever by Sawsan Awad and Daniel Felten. Chapter 27, page: 317-323. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.Incorrect
The correct answer is E.
This patient manifested 2 major Jones criteria: polyarthritis and carditis, thus satisfying criteria for the diagnosis of rheumatic fever and rheumatic heart disease but missing an evidence of GAS infection. That can be documented by detecting an elevated acute phase reactant (ASOT). The time lapse between sore throat and the onset of the symptoms is consistent with the diagnosis of rheumatic fever. The migratory nature of polyarthritis in this patient is consistent with rheumatic fever. Carditis in this patient involves valve lesion (mitral regurgitation), myocardial affliction (poor myocardial function) and pericardial disease (pericardial effusion). Progressive fatigue and enlarged liver are manifestations of heart failure.
Chorea alone, without any other manifestation is satisfactory of diagnosing RF/RHD. Chorea usually is not associated with any other manifestations of RF. SC nodules is another major Jones criteria. Its presence in addition of the already present 2 major jones criteria in this patient is not confirmatory of RF without the presence of elevated acute phase reactant.
Skin rash in general is not diagnostic for RF. The particular rash of RF is the erythema marginatum. Even if this is present, as the SC nodules cannot complete the diagnosis of RF without elevated acute phase reactant.
Prolonged PR interval on 12 lead ECG together with fever are minor Jones criteria of RF.SOURCE:
Rheumatic Fever by Sawsan Awad and Daniel Felten. Chapter 27, page: 317-323. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011. -
Question 5 of 9
5. Question
1 pointsA 10-yr-old boy collapses while competing in a track meet. Emergency medical technicians diagnose ventricular fibrillation and successfully resuscitated the boy. When he arrives in the Emergency Department, the vital signs are stable. Cardiac exam reveals no murmur, click, gallop, or rub. Past medical history is unremarkable. The most common cause of sudden death in this setting is:
Correct
That is Correct!
The presentation of the patient in the question is typical for few cardiac diseases including HCM, Anomalous coronary artery origin and long QTc syndrome. The most common of them all, by statistics, is HCM. Those patients are usually a symptomatic. There are no striking auscultatory findings during rest. At peak exercise, a significant high gradient develops across the left ventricular outflow tract leading to significant obstruction of the blood through the aortic valve. That affects the coronary perfusion leading to myocardial ischemia and subsequent fatal ventricular arrhythmia. Aortic stenosis is a fixed narrowing of the aortic valve. Patients will present with the systolic ejection murmur of aortic valve stenosis at rest. Anomalous coronary artery origin from pulmonary artery usually presents early in life, around 6 weeks of age. Patients present with shock like picture due to repeated ischemia and left ventricular myocardial infarctions. Myocarditis has a different presentation with significant viral illness prior to decompensation. Finally, Ebstein’s anomaly will not present with sudden collapse in the field and also significant tricuspid valve regurgitation would be auscultated at rest.
SOURCE:
Cardiomyopathy by Zahra Naheed and Laura Torchen. Chapter 31, page: 351-357. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.Incorrect
The correct answer is A.
The presentation of the patient in the question is typical for few cardiac diseases including HCM, Anomalous coronary artery origin and long QTc syndrome. The most common of them all, by statistics, is HCM. Those patients are usually a symptomatic. There are no striking auscultatory findings during rest. At peak exercise, a significant high gradient develops across the left ventricular outflow tract leading to significant obstruction of the blood through the aortic valve. That affects the coronary perfusion leading to myocardial ischemia and subsequent fatal ventricular arrhythmia. Aortic stenosis is a fixed narrowing of the aortic valve. Patients will present with the systolic ejection murmur of aortic valve stenosis at rest. Anomalous coronary artery origin from pulmonary artery usually presents early in life, around 6 weeks of age. Patients present with shock like picture due to repeated ischemia and left ventricular myocardial infarctions. Myocarditis has a different presentation with significant viral illness prior to decompensation. Finally, Ebstein’s anomaly will not present with sudden collapse in the field and also significant tricuspid valve regurgitation would be auscultated at rest.
SOURCE:
Cardiomyopathy by Zahra Naheed and Laura Torchen. Chapter 31, page: 351-357. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011. -
Question 6 of 9
6. Question
1 pointsAn 8 year old male presents with his mother for routine health evaluation maintenance. His mother reports that her husband died suddenly of a myocardial infarction at age 37 and was known to have elevated cholesterol. The boy is quite active and participates in cocker and basketball without cardio respiratory complains. He appears healthy with height and weight in the 50th centile for age. Physical examination is unremarkable except for a few Achilles tendon xanthomas. You obtain a fasting lipid pane, which shows total cholesterol of 340, HDL of 42, LDL of 259, and triglycerides of 88.
What is the best next step in management of this patient?Correct
That is Correct!
Although diet and life style change are usually the gold standard treatment in similar patients, the family history of this young boy adds a higher level of risk of developing early cardiovascular disease. This patient in addition to the diet and life style change requires initiation Statin as a first line medical treatment. The patient will then need hepatic enzymes checked in 1 month, then 6 months after that. As rhabdomyolysis is a rare complication of statin therapy, any new muscle soreness, especially soreness not related to exercise, needs to be taken seriously.
SOURCE:
Obesity and Dyslipidemia by Kathryn Holmes and Jacquelyn Busse. Chapter 37, page: 427-434. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.Incorrect
The correct answer is C.
Although diet and life style change are usually the gold standard treatment in similar patients, the family history of this young boy adds a higher level of risk of developing early cardiovascular disease. This patient in addition to the diet and life style change requires initiation Statin as a first line medical treatment. The patient will then need hepatic enzymes checked in 1 month, then 6 months after that. As rhabdomyolysis is a rare complication of statin therapy, any new muscle soreness, especially soreness not related to exercise, needs to be taken seriously.
SOURCE:
Obesity and Dyslipidemia by Kathryn Holmes and Jacquelyn Busse. Chapter 37, page: 427-434. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011. -
Question 7 of 9
7. Question
1 pointsDuring an ultrasound on a 33-week fetus, an obstetrician noted that the fetal HR ranges from 62-66 bpm. Fetal growth appears normal and no structural cardiac abnormalities are identified. Fetal echocardiography reveals that the fetal atria appear to be contracting at 140bpm, with a ventricular rate of 65 bpm. Of the following, the best next step in the management of this fetus is to:
Correct
That is Correct!
This fetus has a low ventricular late despite normal atrial rate, a picture highly suggestive of complete heart block. Mothers of fetuses with complete heart block should be evaluated for connective tissue disorders, particularly systemic lupus erythematosus (SLE). Mothers with SLE are not always symptomatic. Detection of elevated Anti ro/Anti La (SSA/SSB) antibodies can make the diagnosis of maternal SLE or other form of connective tissue disorder with elevated serum antibodies. Those antibodies get transmitted to the fetus through the placenta, damaging the atrioventricular conduction of the fetal heart and result into complete heart block. Low fetal ventricular heart rate may lead to heart failure and fetal hydrops, particularly when the ventricular rate is below 50 bpm. The patient in the vignette has a ventricular rate of 65 bpm, that is usually tolerated without evidence of fetal hydrops. The best option for this fetus is follow up fetal echocardiography and evaluation for signs of fetal hydrops.
SOURCE:
Al-Kubaisi M, Aly SA, Mohammad Nijres B, Awad S. Hypoplastic Left Heart Syndrome with Congenital Complete Heart Block. Pediatr Cardiol. 2017 May 17. doi: 10.1007/s00246-017-1631-8. [Epub ahead of print] PMID: 28512719Incorrect
The correct answer is E.
This fetus has a low ventricular late despite normal atrial rate, a picture highly suggestive of complete heart block. Mothers of fetuses with complete heart block should be evaluated for connective tissue disorders, particularly systemic lupus erythematosus (SLE). Mothers with SLE are not always symptomatic. Detection of elevated Anti ro/Anti La (SSA/SSB) antibodies can make the diagnosis of maternal SLE or other form of connective tissue disorder with elevated serum antibodies. Those antibodies get transmitted to the fetus through the placenta, damaging the atrioventricular conduction of the fetal heart and result into complete heart block. Low fetal ventricular heart rate may lead to heart failure and fetal hydrops, particularly when the ventricular rate is below 50 bpm. The patient in the vignette has a ventricular rate of 65 bpm, that is usually tolerated without evidence of fetal hydrops. The best option for this fetus is follow up fetal echocardiography and evaluation for signs of fetal hydrops.
SOURCE:
Al-Kubaisi M, Aly SA, Mohammad Nijres B, Awad S. Hypoplastic Left Heart Syndrome with Congenital Complete Heart Block. Pediatr Cardiol. 2017 May 17. doi: 10.1007/s00246-017-1631-8. [Epub ahead of print] PMID: 28512719 -
Question 8 of 9
8. Question
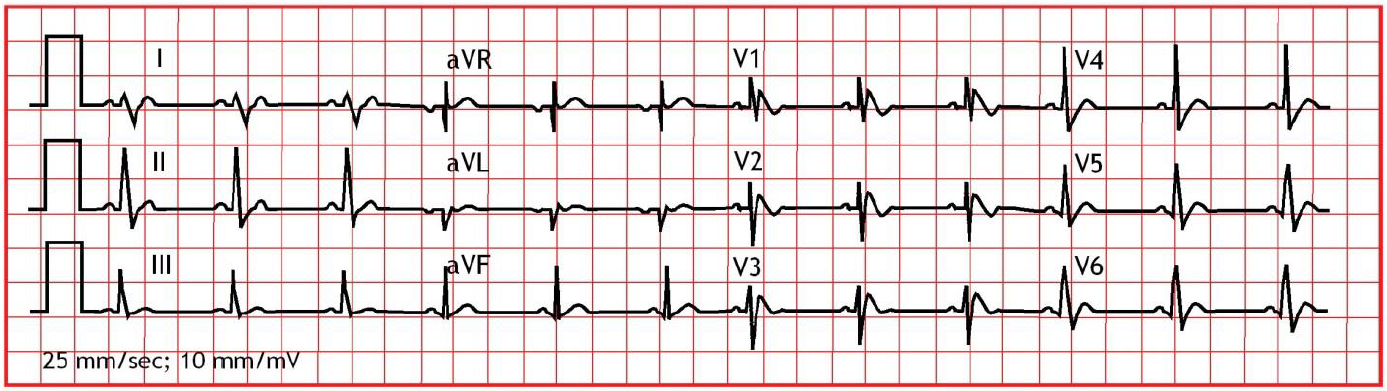
1 pointsA 2year old boy with a large ASD and hypertrophied muscle bundles in the right ventricular outflow tract with minimal obstruction. Physical examination was remarkable for a 3/6 systolic flow murmur in the left upper sternal border and a 2/4 mid-diastolic murmur in the left lower sternal border. S2 was split without variation throughout the respiratory cycle. Surgical closure of the ASD and resection of hypertrophied muscle bundles was performed. Physical examination post-operatively indicates no residual murmur; however, S2 continues to have fixed splitting through-out the respiratory cycle. ECG is shown below.
What is causing the fixed splitting of S2 post-operatively?
Correct
That is Correct!
Fixed splitting of second heart sound in patients with ASD is caused by the constant delay in closure of the pulmonary valve due to excessive blood flow through it as a result of the ASD. Once the ASD is closed, murmurs and fixed splitting of the second heart sound should be resolved. Another cause for fixed splitting of the second heart sound is delayed start of RV contractility in systole, such as with right bundle branch block, this will cause delay in pulmonary closure throughout the respiratory cycle.
This patient underwent closure of ASD as well as resection of hypertrophied muscle bundles. The former caused the resolution of murmurs, however, the latter could cause right bundle branch block which is seen in the ECG. This will also cause delayed closure of the pulmonary valve, due to a different mechanism, resulting in continuation of fixed splitting of the second heart sound.SOURCE:
Atrial Septal Defect by Ra-id Abdulla and Austin Hanrahan. Chapter 6, page: 91-102. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.Incorrect
Correct answer is C.
Fixed splitting of second heart sound in patients with ASD is caused by the constant delay in closure of the pulmonary valve due to excessive blood flow through it as a result of the ASD. Once the ASD is closed, murmurs and fixed splitting of the second heart sound should be resolved. Another cause for fixed splitting of the second heart sound is delayed start of RV contractility in systole, such as with right bundle branch block, this will cause delay in pulmonary closure throughout the respiratory cycle.
This patient underwent closure of ASD as well as resection of hypertrophied muscle bundles. The former caused the resolution of murmurs, however, the latter could cause right bundle branch block which is seen in the ECG. This will also cause delayed closure of the pulmonary valve, due to a different mechanism, resulting in continuation of fixed splitting of the second heart sound.SOURCE:
Atrial Septal Defect by Ra-id Abdulla and Austin Hanrahan. Chapter 6, page: 91-102. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011. -
-
Question 9 of 9
9. Question
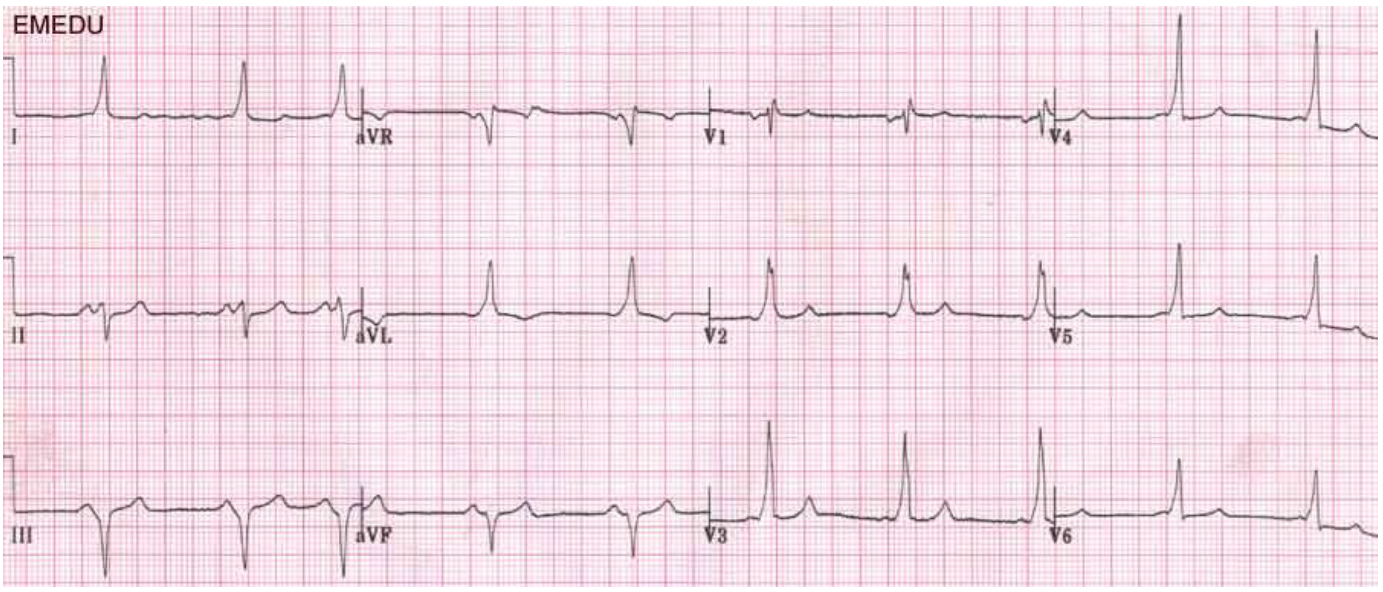
1 pointsCorrect
That is Correct!
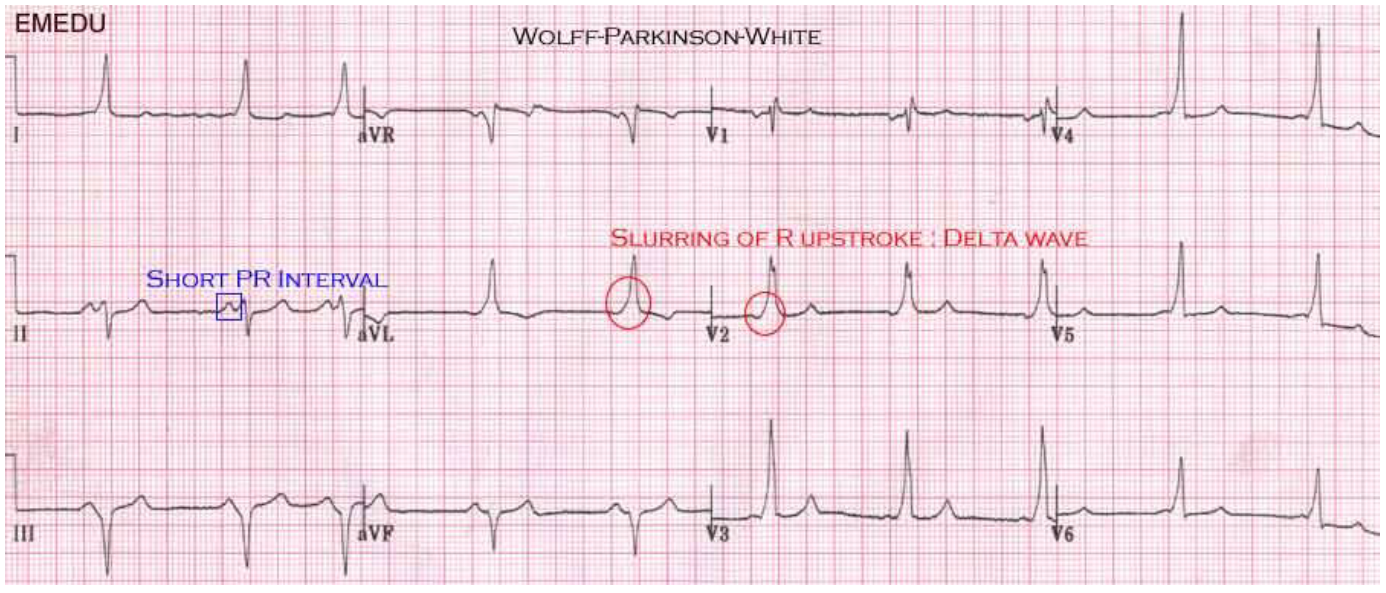
NQ6-Exp
The ECG is a classic presentation of WPW syndrome. The short PR interval and the Slurring of the R wave upstroke together with widening of the base of the QRS (secondary the Slurring of the R wave upstroke) are all criteria of WPW syndrome. This is common re-entry tachycardia. There is an accessory pathway, usually to the left of the AVN. Patients usually presents with supraventricular tachycardia and congestive heart failure. The definite treatment of the WPW syndrome is ablation around teen age.
SOURCE:
Cardiac Arrhythmias by William Bonney and Ra-id Abdulla. Chapter 32, page: 359-383. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.Incorrect
Correct Answer is D
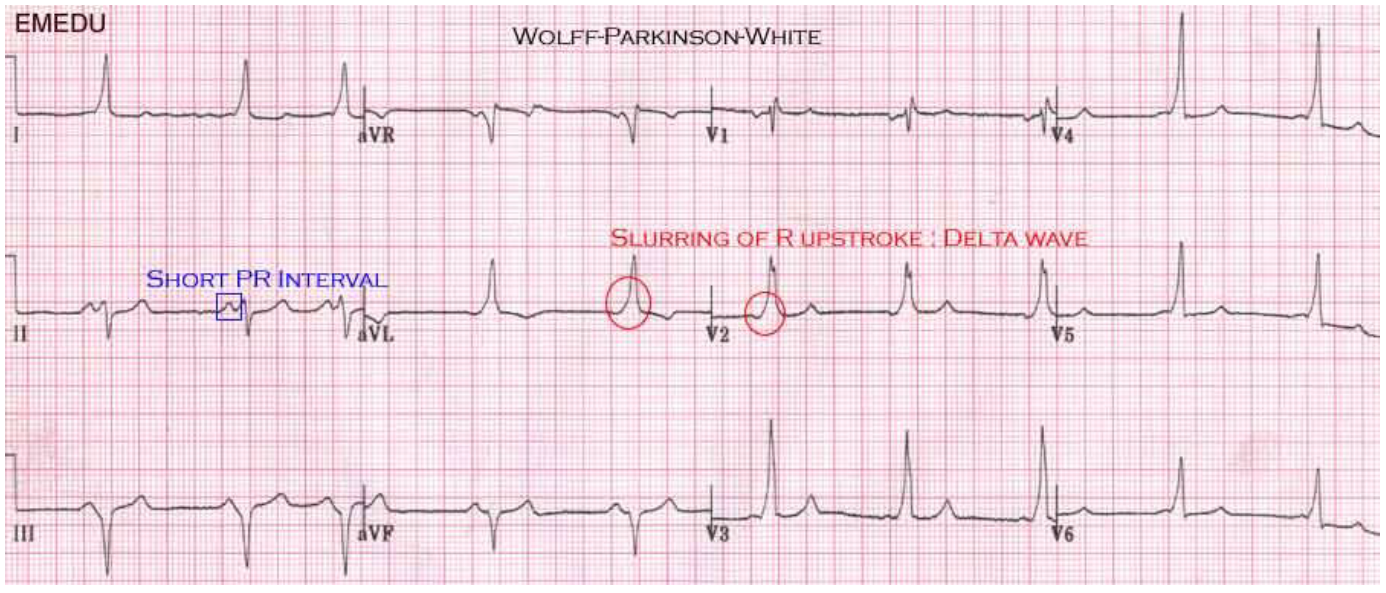
NQ6-Exp
The ECG is a classic presentation of WPW syndrome. The short PR interval and the Slurring of the R wave upstroke together with widening of the base of the QRS (secondary the Slurring of the R wave upstroke) are all criteria of WPW syndrome. This is common re-entry tachycardia. There is an accessory pathway, usually to the left of the AVN. Patients usually presents with supraventricular tachycardia and congestive heart failure. The definite treatment of the WPW syndrome is ablation around teen age.
SOURCE:
Cardiac Arrhythmias by William Bonney and Ra-id Abdulla. Chapter 32, page: 359-383. In Heart Diseases in Children. Ed. Ra-id Abdulla Springer Science and Business Media LLC 2011.